Abstract
BACKGROUND: Therapy-related myeloid neoplasms (t-MN) develop after exposure to a variety of DNA-damaging agents including chemotherapy, radiation, and immunosuppressive therapies (IST). Recently, a cohort of radiation t-MN (Rt-MN) was described (Patel et al, Blood Adv, 2022). Most common cytogenetic and genetic abnormalities were that of chromosomes 5 and 7, and ASXL1 and TET2 mutations. However, only a smaller subset (n=16) underwent next-generation sequencing (NGS) analysis and comparison of clinicopathological features and outcomes with other forms of DNA-damaging therapies was not performed. We hypothesized that Rt-MN may have different clinicopathological features and outcomes compared to t-MN after other forms of therapy.
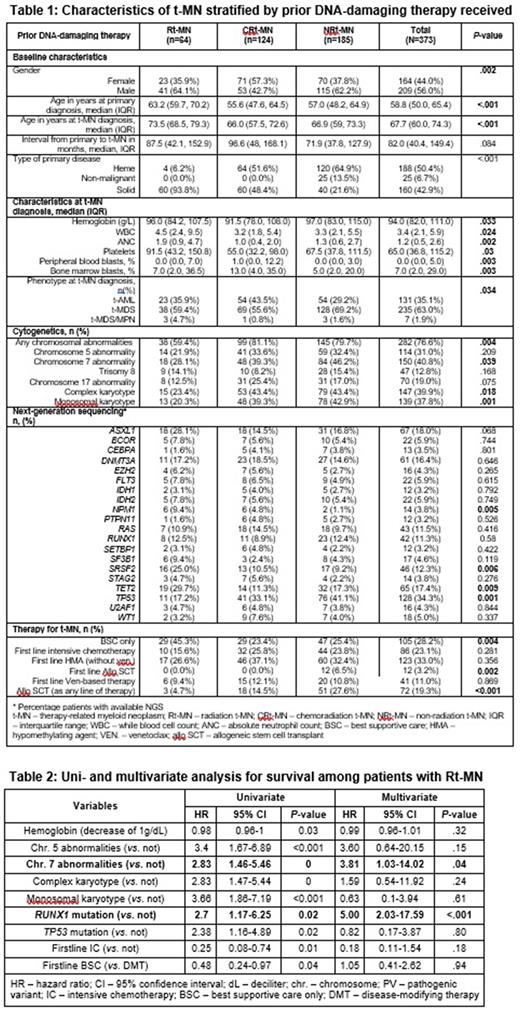
METHODS: This retrospective, multicenter study was conducted at Mayo Clinic, Rochester (USA) and South Australian Local Health Network (South Australia, Australia). Following appropriate regulatory approvals at the respective institute, we identified 373 WHO-defined t-MN patients who had cytogenetics and NGS at t-MN diagnosis.
The statistical analysis for continuous and categorical variables was performed using Mann-Whitney and chi-squared tests, respectively. Overall survival (OS) was calculated from the time of t-MN diagnosis to the last follow up or death, whichever came first using Kaplan-Meier method. Uni- and multivariate analyses were performed using Cox proportional hazard model. The statistical analysis was performed using BlueSky (Chicago, IL, USA).
RESULTS: Sixty-four (17.2%) patients developed Rt-MN and 124 (33.2%) following chemoradiotherapy (chemoradiation t-MN or CRt-MN). The remaining 185 (49.6%) received chemotherapy and/or IST but did not receive radiation (non-radiation t-MN or NRt-MN).
1. Clinical characteristics: Rt-MN were significantly older at the time of primary diagnoses (Table 1) and presented with a higher median white blood cell count, absolute neutrophil count, and platelets. A significantly higher proportion of Rt-MN patients had solid primary malignancy compared to CRt-MN and NRt-MN (P<.001).
2. Biological characteristics: The proportion of patients with chromosome 5 and 7 abnormalities was significantly lower in Rt-MN patients and comparable to the previously described cohort. Similarly, a significantly lower proportion of Rt-MN patients had evidence of genomic instability in the form of complex karyotype (CK; P=.018) and monosomal karyotype (MK; P=.001) compared to CRt-MN and NRt-MN. Rt-MN was enriched in mutated SRSF2 (P=0.006), TET2 (P=.009) and NPM1 (P=.005) compared to CRt-MN and NRt-MN respectively. On the other hand, Rt-MN had a significantly lower proportion of TP53mut compared to CRt-MN and NRt-MN (P=.001).
3. Outcomes after t-MN diagnosis: Although a significantly higher proportion of Rt-MN patients received best supportive care only (P=0.004), median OS from the time of t-MN diagnosis was not different between for Rt-MN, CRt-MN, and NR-tMN (12 vs. 12.3 vs. 15 months, respectively; P=0.11). After a median follow up of 47 months, 288 (77.2%) patients died. Interestingly, among Rt-MN patients, receiving FL HMA was associated with an inferior survival compared to those receiving BSC or IC (HMA 11 mo., BSC 18 mo., and IC 73 mo., P=.01).
4. Factors predicting survival of Rt-MN patients: Univariate analysis identified hemoglobin, chromosome 5 and 7 abnormalities, CK, MK, RUNX1 and TP53 mutations, and the type of first line therapy as predictors of survival (Table 2). MVA that included the above factors, age, and type of primary disease identified RUNX1 mutation (median OS 6 mo. vs. 13 mo., P=.02) and chromosome 7 abnormalities (7.8 mo. vs. 19.4 mo., P<0.001) as independent variables for OS.
CONCLUSIONS: While Rt-MN less frequently harbored the traditionally high-risk features including CK, MK, and TP53 mutation, and were less likely to receive disease-modifying therapies, survival was not different from the patients who received the other forms of DNA-damaging therapies. Possible explanations of the noted discrepancy include older age at t-MN diagnosis and under-utilization of disease-modifying therapies. IC treatment of Rt-MN appears to be associated with a favorable OS. The presence of mutated RUNX1 and chromosome 7 abnormalities are independent risk factors for survival in Rt-MN patients. In summary, Rt-MN is a distinct clinical and molecular entity within the heterogeneous t-MN category.
Disclosures
Al-Kali:Astex: Other: research support to institution. Patnaik:Kura Oncology, Stemline Therapeutics: Research Funding. Hiwase:BMS: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Speakers Bureau; AbbVie: Speakers Bureau. Shah:Astellas: Research Funding; Celgene: Research Funding; Marker Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal